Sphenopalatine Block for Pain Management
Facial pain affects around 25% of the adult population. It can be caused by inflammatory illnesses and infections such as toothache and diseases affecting the facial bone, paranasal sinuses, and salivary glands, as well facial neuralgias such as cluster headaches, acute migraine, trigeminal (V1 ophthalmic and V2 maxillary) neuralgia, and sphenopalatine neuralgia. Unfortunately, facial pain exhibits limited or no positive response to physical therapy and often requires the administration of high-dosage medications. To effectively treat facial pain, the sphenopalatine ganglion (SPG) block has been administered to patients with a 50% success rate reported by multiple studies.
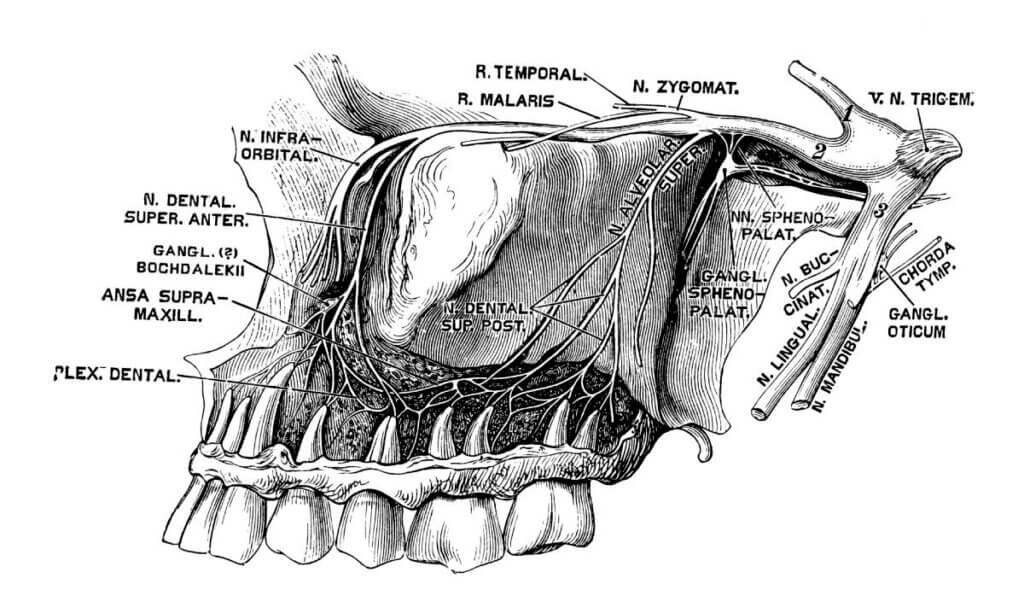
The sphenopalatine block can inhibit the somatic sensory afferent fibers of the trigeminal nerve and the post-ganglionic sympathetic neurons since they both pass through the ganglion. Blocking the sphenopalatine ganglion relieves facial pain because it interrupts the nociception process. There are three methods for performing SPG block: trans-oral, lateral, and trans-nasal. Among these, the trans-nasal route is considered the easiest and best tolerated. 3
A study conducted by Schaffer et al. investigated the effectiveness of sphenopalatine block using bupivacaine by comparing it to an injection of saline solution in patients with headaches. The findings indicated no significant difference between the bupivacaine and saline solution cohorts. After 15 minutes, both cohorts experienced a 50% reduction in discomfort. After 24 hours, a higher proportion of patients in the bupivacaine group experienced relief compared to those who received the saline solution. Similarly, a study by Jespersen et al. found no statistically significant disparity in pain perception between individuals who underwent a block using a solution of lidocaine 4% and ropivacaine 0.5% in a 1:1 ratio and those who received saline. To explain this statistic, Jespersen et al. argue that relief might be achieved due to mechanical stimulation and not anesthesia of the nerve; however, researchers remain uncertain about the mechanism of the block. Jespersen et al. also did not rule out the possibility that saline may have a therapeutic effect. Their results showed a 60% (12/20) reduction in pain in the patients who were administered the anesthetic, compared to 45% (9/20) for those who got saline.3,2
Another study by Candido et al. examined pain alleviation utilizing their FDA-approved Tx360® nasal applicator for medication delivery. They created a trans-nasal, needle-free, topical method for administering sphenopalatine block. The width of the spray diffusion is designed to be large enough to accommodate the anatomical diversity of the sphenopalatine foramen (SPF). The three patients in their study reported long-lasting pain relief, though a larger sample size in future research will be critical.4
Blocking pain over a period of time may be more effective in thoroughly breaking the pain cycle by causing a longer-lasting change in the autonomic nervous system. This may offer extended durations of pain relief or, in certain instances, a total cessation of chronic symptoms.4 Additional research to explain the mechanism of pain relief behind a sphenopalatine block and the variation in block outcomes will improve the understanding and treatment of facial pain.
References
- Zanella, Simone, et al. “Transnasal Sphenopalatine Ganglion Blockade for Acute Facial Pain: A Prospective Randomized Case-control Study.” PubMed, vol. 22, no. 1, Jan. 2018, pp. 210–16, doi:26355/eurrev_201801_14119.
- Schaffer, Jason T., et al. “Noninvasive Sphenopalatine Ganglion Block for Acute Headache in the Emergency Department: A Randomized Placebo-Controlled Trial.” Annals of Emergency Medicine, vol. 65, no. 5, May 2015, pp. 503–10, doi:1016/j.annemergmed.2014.12.012.
- Jespersen, Mads Seit, et al. “Sphenopalatine Ganglion Block for the Treatment of Postdural Puncture Headache: A Randomised, Blinded, Clinical Trial.” British Journal of Anaesthesia, vol. 124, no. 6, June 2020, pp. 739–47, doi:1016/j.bja.2020.02.025.
- Candido, Kenneth D. “A Novel Revision to the Classical Transnasal Topical Sphenopalatine Ganglion Block for the Treatment of Headache and Facial Pain.” Pain Physician, vol. 6;16, no. 6;11, Nov. 2013, pp. E769–78, doi:36076/ppj.2013/16/e769.



