Components of a Spinal Kit in Anesthesia
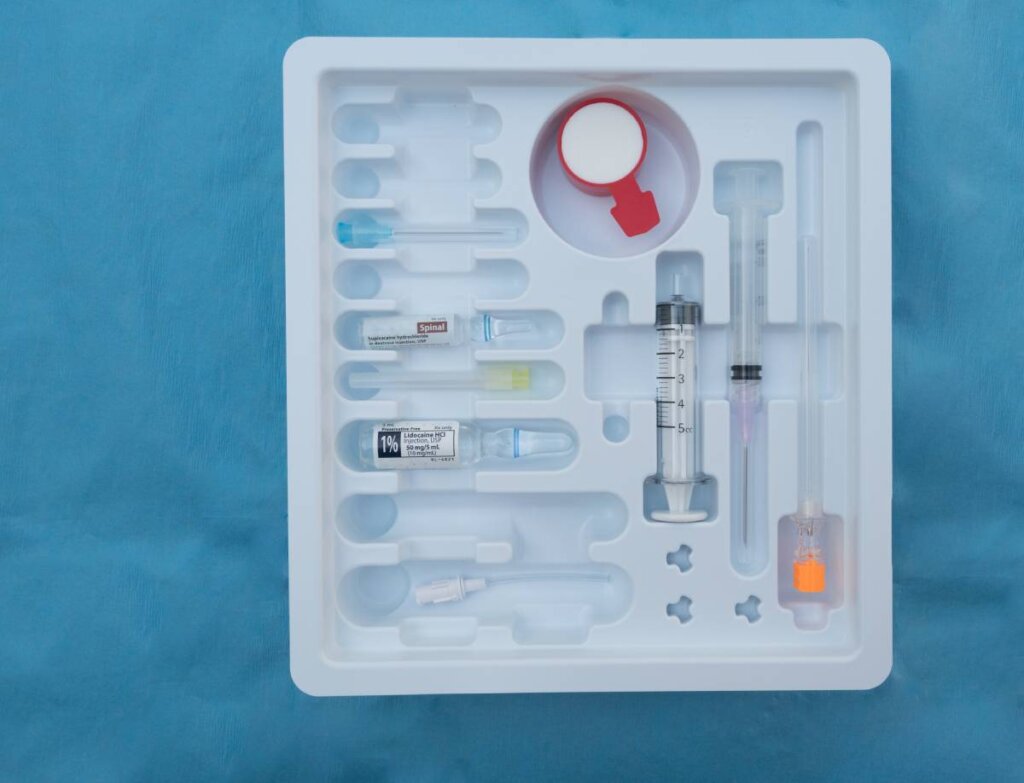
A spinal kit in anesthesia is intended to be a one-stop shop of equipment for the administration of spinal anesthesia, a procedure commonly used for surgeries involving the lower abdomen, pelvis, and lower limbs. The components of a spinal kit should contain everything necessary for achieving the optimal outcome, ensuring patient safety, and minimizing complications 1.
The spinal needle is the primary instrument used to deliver the anesthetic agent into the subarachnoid space, where cerebrospinal fluid surrounds the spinal cord. These needles are specifically designed to be thinner, longer, and with a sharp bevel for easier insertion compared to other needles used in anesthesia. They often come with markings to indicate the depth of insertion, providing an accurate way to position the needle—the most commonly used needles are the 25 to 27 gauge, with a longer needle for adults and a shorter one for children or smaller individuals 2,3.
A local anesthetic like bupivacaine, lidocaine, or ropivacaine is injected into the subarachnoid space through the spinal needle. The selection of the anesthetic solution depends on the type and duration of the surgery and the desired level of anesthesia. Sometimes, opioids like morphine or fentanyl are added to enhance the analgesic effect and extend the duration of the block 4,5.
A sterile syringe – used to draw and inject the anesthetic solution – is one of the necessary components of a spinal kit. The syringe is often pre-filled or prepared by the anesthesia provider in a sterile environment to prevent contamination; volume and concentration of the anesthetic are carefully measured to avoid overdose and ensure a precise block level.
A scalpel may be included in the kit to make a small incision in the skin if necessary. This incision is usually very minimal and carried out to facilitate the placement of the spinal needle, particularly in cases where there is difficulty locating the target area for injection.
Sterile drapes are used to cover the surgical site, ensuring the area around the injection site remains sterile. These drapes are essential in preventing infection by maintaining a clean and controlled environment throughout the procedure—they are typically made from non-woven materials that are resistant to contamination. Sterile gloves are also essential for maintaining a sterile field during the procedure. The anesthesia provider wears gloves to avoid contamination and to protect both the patient and themselves from potential infections.
In some cases, a local anesthetic such as lidocaine is injected just under the skin to minimize pain during the insertion of the spinal needle, ensuring the patient is comfortable and reduces the anxiety often associated with the procedure 6,7.
Beyond the components of a spinal kit, monitoring equipment is vital during the procedure. This includes devices for monitoring blood pressure, heart rate, oxygen saturation, and respiratory rate. These vital signs are monitored throughout the procedure and into the recovery phase to ensure patient stability 8.
A spinal anesthesia kit contains several key components that help the anesthesia provider achieve safe and effective anesthesia for patients undergoing surgery. However, even if spinal kits are not available, a facility performing spinal anesthesia must have all the aforementioned equipment available.
References
1. Operater. Spinal Anesthesia. NYSORA https://www.nysora.com/techniques/spinal-anesthesia-2/ (2018).
2. Kang, S. B. et al. Comparison of 26- and 27-G needles for spinal anesthesia for ambulatory surgery patients. Anesthesiology 76, 734–738 (1992). DOI: 10.1097/00000542-199205000-00011
3. Types of Anaesthesia Needles – Medical Devices. https://www.medicaldevices.co.uk/anaesthesia-needles-and-their-types/.
4. Dull, R. O. & Peterfreund, R. A. Variations in the composition of spinal anesthetic solutions: the effects of drug addition order and preparation methods. Anesth Analg 87, 1326–1330 (1998). DOI: 10.1097/00000539-199812000-00021
5. Imbelloni, L., Gouvei, M. & de Lemos Neto SV. Spinal anesthesia, puncture position and local anesthetic solutions. Better understanding for better indication. Journal of Anesthesia & Critical Care: Open Access (2023). DOI: 10.15406/jaccoa.2023.15.00566
6. Rękas-Dudziak, A., Męcińska-Jundziłł, K., Walkowiak, K. & Witmanowski, H. The use of local anaesthetics in dermatology, aesthetic medicine and plastic surgery: review of the literature. Postepy Dermatol Alergol 40, 22–27 (2023). doi: 10.5114/ada.2023.125221
7. Woolfson, A. D. & McCafferty, D. F. Local anaesthesia of the skin. J Clin Pharm Ther 14, 103–109 (1989). DOI: 10.1111/j.1365-2710.1989.tb00228.x
8. NYSORA. Equipment for Regional Anesthesia. NYSORA https://www.nysora.com/topics/equipment/equipment-regional-anesthesia/ (2018).



