Opioid Pain Management in Pediatric Surgical Patients
Opioid pain management in pediatric surgical patients is a complex endeavor that requires careful consideration of various factors to ensure effective pain relief while minimizing risks. Opioids are commonly used to manage moderate to severe postoperative pain when alternative methods are unlikely to provide adequate analgesia. However, their use necessitates a nuanced approach, considering dosing precautions, monitoring strategies, potential side effects, and regulatory considerations.1
Dosing precautions are paramount when initiating opioid therapy for pain management in pediatric patients. Healthcare professionals must start with low doses and adjust them incrementally based on individual patient response. This approach is particularly crucial in the early phases of postoperative care until an effective dose is established. Factors such as age, prematurity, and underlying medical conditions must be considered when determining opioid doses.
Concurrent administration of opioids with other respiratory depressants should be managed cautiously to minimize the risk of adverse respiratory events.2 High-risk patients, especially those with pre-existing neurologic impairment, may require dose adjustments and close monitoring to prevent complications.
Vigilant monitoring during opioid administration is critical to detect and address potential adverse effects promptly. Regular assessment of respiratory rate, sedation level, and oxygen saturation is essential to ensure patient safety. Clinical assessment tools such as the modified Pasero Opioid Induced Sedation Scale (m-POSS) can aid in identifying sedation levels and guiding interventions appropriately.3 Moreover, proactive measures to manage opioid-related side effects, including nausea, pruritus, and constipation, are essential for improving patient comfort and adherence to pain management regimens.
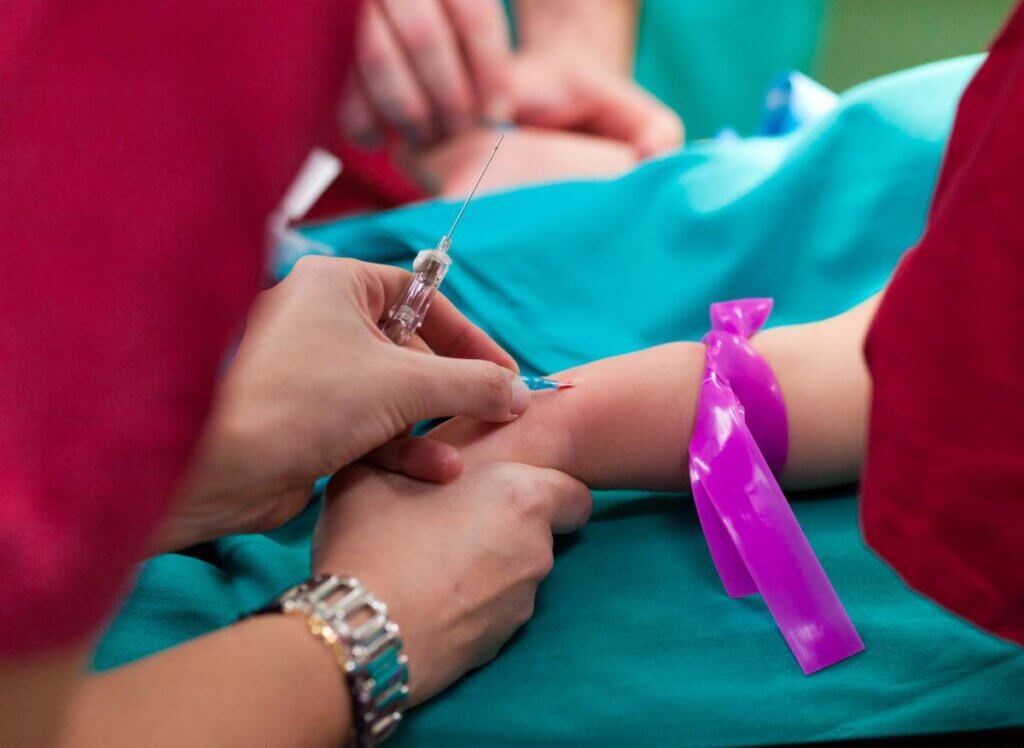
Parenteral opioids, such as morphine, hydromorphone, and fentanyl, offer rapid pain relief but require particularly careful dosing to prevent adverse effects. Bolus IV injections are commonly used for moderate pain, with doses tailored to individual needs. Patient-controlled analgesia (PCA) represents a valuable modality for self-administration of opioid medication in cooperative pediatric patients, allowing for timely access to analgesia and empowering patients in pain management decisions.4
Transitioning to oral opioids is typically favored as patients progress in their recovery, promoting mobility and minimizing reliance on parenteral administration. Immediate-release opioids are preferred for acute pain management, allowing for flexible dosing adjustments. Post-discharge, a multimodal approach to pain management is advocated, incorporating nonpharmacologic interventions alongside acetaminophen and NSAIDs. Opioids are prescribed cautiously, with an emphasis on limiting duration and quantity to mitigate the risk of misuse.
Postoperative opioid medication in pediatric patients poses a risk of prolonged opioid use and contributes to the broader opioid epidemic. Despite efforts to reduce postoperative opioid prescriptions, significant variations in prescribing practices in pediatric settings persist. A survey conducted among pediatric surgeons, PACU nurses, and surgical residents revealed notable differences in beliefs and practices regarding pediatric postoperative opioid requirements. While pediatric surgeons generally aligned with evidence supporting opioid-free postoperative pain management, surgical residents and PACU nurses tended to estimate longer durations for opioid needs, particularly for teenagers at higher risk of opioid abuse. This underscores the importance of targeted educational interventions involving all stakeholders to promote multimodal pain management approaches and mitigate opioid usage in pediatric surgical patients.5
In conclusion, effective opioid pain management in pediatric surgical patients requires a comprehensive and individualized approach. By adopting a tailored approach to each patient’s needs and closely monitoring their response to treatment, healthcare professionals can optimize pain control while minimizing the risk of adverse effects. Continued research and clinical vigilance are essential for refining opioid management practices and improving outcomes in pediatric surgical care.
References
- Kelley-Quon, Lorraine I., et al. “Guidelines for Opioid Prescribing in Children and Adolescents after Surgery: An Expert Panel Opinion.” JAMA Surgery, vol. 156, no. 1, 1 Jan. 2021, pp. 76–90, jamanetwork.com/journals/jamasurgery/fullarticle/2772855, https://doi.org/10.1001/jamasurg.2020.5045.
- Jungquist, Carla R., et al. “American Society for Pain Management Nursing Guidelines on Monitoring for Opioid-Induced Advancing Sedation and Respiratory Depression: Revisions.” Pain Management Nursing, vol. 21, no. 1, Feb. 2020, pp. 7–25, https://doi.org/10.1016/j.pmn.2019.06.007.
- Pasero, Chris. “Assessment of Sedation during Opioid Administration for Pain Management.” Journal of PeriAnesthesia Nursing, vol. 24, no. 3, June 2009, pp. 186–190, https://doi.org/10.1016/j.jopan.2009.03.005.
- Berde, Charles B, et al. “Patient-Controlled Analgesia in Children and Adolescents: A Randomized, Prospective Comparison with Intramuscular Administration of Morphine for Postoperative Analgesia.” The Journal of Pediatrics, vol. 118, no. 3, 1 Mar. 1991, pp. 460–466, https://doi.org/10.1016/s0022-3476(05)82169-9.
- Stokes, Sarah C., et al. “Variations in Perceptions of Postoperative Opioid Need for Pediatric Surgical Patients.” JAMA Surgery, vol. 156, no. 9, 1 Sept. 2021, p. 885, https://doi.org/10.1001/jamasurg.2021.2076.



